Let’s talk about myelin
To stop MS, we need treatments that repair damage to the protective myelin coating around nerves.
Last updated: 30th September 2022
What’s on this page?
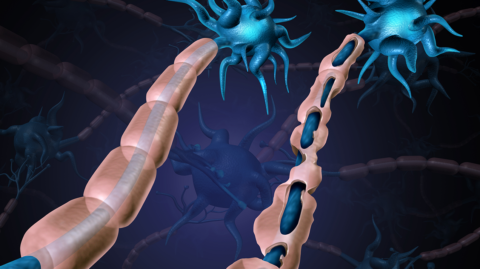
Illustration of nerve cell and myelin
Nerve cells carry messages between the brain and spinal cord and the organs and limbs of the body. They control everything we do, from how we move to how we think and feel.
Myelin is the fatty protective coating that surrounds nerve fibres – a bit like the insulation on an electrical wire.
As well as protecting the fragile nerve fibres, myelin also allows messages to travel quickly along the nerves without being lost or interrupted.
As well as protecting the fragile nerve fibres, myelin also allows messages to travel quickly along the nerves without being lost or interrupted.
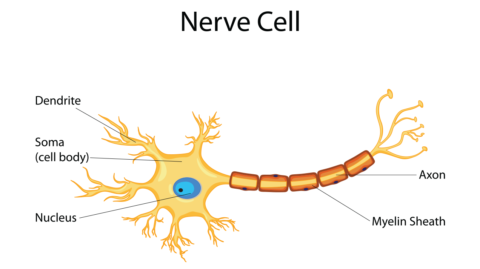
Diagram of a nerve cell identifying myelin
What happens to myelin in MS?
In MS, immune cells enter the brain and spinal cord and attack both the myelin and the cells that make it. When myelin becomes damaged, messages find it harder to get through – or can’t get through at all. That’s what causes the symptoms of MS.
These symptoms can be very different for people, depending on where in the brain and spinal cord the attack has occurred.
Why do we need to repair myelin?
If myelin isn’t repaired properly, the nerve fibres become increasingly vulnerable to damage. And over time they may be lost. When this happens, messages can no longer get through and symptoms become permanent.
This gradual, steady accumulation of disability is what we call MS progression. It’s why we need to find ways to put myelin back on nerves, protecting them from damage and getting the messages flowing again.
How can we repair and replace myelin?
The human body has an amazing natural ability to repair myelin and get nerves working properly again.
Myelin is repaired or replaced by special cells in the brain called oligodendrocytes. These cells are made from a type of stem cell found in the brain, called oligodendrocyte precursor cells (OPCs).
- Nerve cells signal for help when their myelin is damaged
- When the signal reaches the OPCs, they travel to the site of damage and mature into oligodendrocytes
- At that point, the damage can be repaired
Early in the condition, this process works quite well. With the myelin replaced, the messages are able to travel down the nerve fibre again. Your MS symptoms may lessen or go away as the immune attack subsides.
But, with age and repeated attacks, this process stops working as effectively. It’s thought that OPCs stop responding to the nerve cells’ cry for help, and damaged oligodendrocytes can no longer effectively replace the lost myelin.
We need to find ways to kickstart this natural process again. This involves understanding everything about the process: from how nerve cells signal for help, to finding out what molecules help activate the myelin-making cells. Researchers then have to translate these findings into developing treatments that will help people with both relapsing and progressive MS.
This is no small task but we’re making good progress.
Myelin repair research in the pipeline
The global MS community is working on some interesting research on myelin repair. We outline two of these investigations below:
What role does the protein called SphK2 play in remyelination?
Some DMTs, like fingolimod and siponimod used to treat progressive MS, are called Sphingosine-1-phosphate receptor modulators (S1P). S1P reduces inflammation in MS, and may also help repair damaged myelin. A study funded by MS Australia is investigating a protein called SphK2 that produces S1P in the brain.
Early work shows that SphK2 plays a role in maintaining myelin with age, and may also help the brain in preserving its oligodendrocytes, which are crucial for myelination. The same group is now researching whether treatments that modulate S1P levels, like fingolimod and siponimod, protect myelin from degenerating and promote remyelination.
What role does temelimab play in remyelination?
An international clinical trial is investigating the safety and impact of temelimab on myelination. Temelimab is an antibody treatment that targets a virus called MSRV-Env. MSRV-Env is sometimes active in people with MS, and may be responsible for the immune response triggering myelin breakdown.
Early results show that temelimab may promote remyelination and prevent loss of nerves, but does not affect MS inflammation. This work is being followed up in another study, testing the effect of temelimab with a wider dose range, following treatment with rituximab.
With thanks to the UK MS Society who shared this original article with us.